ACA Reporting
Hello again,
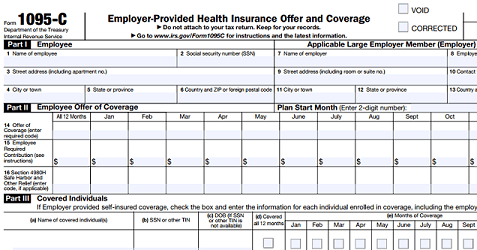
This post is for Applicable Large Employers (ALEs) required to comply with the Affordable Care Act. We hope you find this helpful for your ACA Reporting.
The following information is quoted from hni.com:
Affordable Healthcare Defined for ALEs
ALEs must offer their eligible full-time employees health insurance that provides minimum essential coverage (MEC) that is both affordable and provides minimum value (actuarial value of at least 60%).
Employers need to offer coverage to at least 95% of their eligible full-time employees in their workforce.
Health care coverage is deemed to be affordable if the employee’s required contribution for the lowest cost self-only health insurance option offered by the employer is 9.5% (indexed annually) or less of the employee’s household income.
This applies even if the employee selects a different health insurance coverage option.
Safe Harbors for Employers
Under the ACA, there are three safe harbors that employers could use to demonstrate compliance with the affordability standard, all of which are calculated to the cost of the lowest employee self-only coverage made available to all eligible employees.
These three safe harbor affordability standards remain unchanged from prior years and are:
- Form W-2 Safe Harbor (based on the employee’s W-2, Box 1 reported wages for that year),
- Rate of Pay Safe Harbor (based on an employee’s hourly rate times 130 hours per calendar month), or
- Federal Poverty Line Safe Harbor (based on the annual federal poverty line for a single individual divided by 12).
Income Affordability Standard
This 9.5% income affordability standard has been adjusted upwards the past two years. The annual adjustment for 2016 was 9.66% and the adjustment for 2017 was 9.69%. However, for purposes of the employer shared responsibility mandate, the required contribution percentage will be decreased for 2018 to 9.56%.
This means that if an employee’s share of the premium (in 2018) for the lowest cost self-only option offered by the employer is more than 9.56% of his or her household income, the coverage is not considered affordable for that employee and the ALE member may be liable for a penalty if that employee obtains a premium tax credit for health coverage purchased through the marketplace.
Pay or Play Mandate
The original $2,000 amount associated with the section 4980H(a) penalty (failure to offer coverage to 95% of eligible full-time employees with MEC) and the original $3,000 amount associated with the section 4980H(b) penalty (failure to offer affordable coverage) have been adjusted each calendar year beginning after 2014.
In 2016, these numbers were $2,160 and $3,240 respectively and in 2017, these penalties are $2,260 and $3,390. The adjusted numbers to use in 2018 for a section 4980H(a) penalty amount is $2,320 and a section 4980H(b) penalty amount will be $3,480.
For questions about ACA reporting and compliance Contact Us. Or, learn more about how our ACA Reporting Software can help you simplify reporting and compliance year-round.
